In some cases, when a second incision around the anus is made, some of the skin and soft tissue will need to be removed at that time. Mr Chattopadhyay usually asks a plastic surgeon to be involved in the operation to repair the changes made by the surgery. The plastic surgeon may use what is known as a ‘flap’ to make the repair.
Agreeing to treatment
Mr Chattopadhyay will ask you to sign a consent form agreeing to accept the treatment that you are being offered. The basis of the agreement is that you have understood the proposed treatment and that you have been given an opportunity to discuss any concerns.
Benefits and risks of surgery
Benefits of surgery
The intended benefits of surgery are to remove the cancer and to relieve any symptoms you may be experiencing as a result of the cancer. The long-term benefits depend on the extent to which the cancer can be removed.
What happens if I do not have surgery?
If you decide not to have surgery, the cancer will continue to grow and your symptoms may get worse. Mr Chattopadhyay will discuss this with you, and if appropriate will discuss other treatments that may be suitable for you such as chemotherapy.
Are there any alternatives to an operation?
Yes, but these vary from patient to patient. Surgery is thought to be the best form of treatment to remove this type of cancer. However, if you decide not to go ahead with surgery, chemotherapy may be suitable for you. Alternatively, you could opt for a ‘watch and wait’ policy; this involves deciding on a treatment plan for controlling your symptoms. Mr Chattopadhyay will discuss with you the best form of treatment for you.
Common risks of surgery
This is a major operation and, as with any form of surgery, problems can occur. Common risks of surgery include:
- chest infection (particularly if you are a smoker)
- wound infection
- urine infection
- bleeding and the need for a blood transfusion
- blood clot in the leg (DVT or deep vein thrombosis)
- Frequently the bowels can be slow to start working again. This requires patience but usually resolves in time (this is known as an ileus).
Steps will be taken to minimise the risks of surgery such as giving you TEDs (thromboembolic deterrent stockings) which are special elastic stockings, to wear and giving you blood-thinning injections to prevent DVT.
Less common risks of surgery include:
- post operative bleeding (haemorrhage)
- heart attack (myocardial infarction)
- blood clot in the chest (pulmonary embolism)
- formation of internal scarring (adhesions)
- risk of the wound opening up, wound breakdown or skin flap failure
- Incomplete removal of the cancer or none of the cancer being removable.
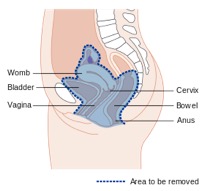
How will total pelvic clearance surgery affect me?
Stoma formation
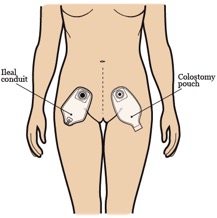
As your bladder and lower bowel (colon) are removed during surgery, you will no longer be able to sit on the toilet to pass urine and faeces in the usual way. During your operation you will have two stomas created, one for your faeces and wind (colostomy) and a second for your urine (urostomy). The word stoma comes from the Greek, meaning mouth or opening. It is moist, pinky red in colour, and similar to the inside of your mouth. The stoma itself has no feeling, but has a good blood supply, and will protrude slightly on the surface on your abdomen to allow the drainage of waste (urine and faeces) into a bag.
Colostomy
Part of your bowel (colon and rectum) will be removed during your operation, and the upper end will be brought out on to the skin surface to create your colostomy. A colostomy is usually on the left hand side of your abdomen. A bag sticks over the colostomy to collect your faeces and wind. The remaining lower end of your bowel may need to be removed, and if so your back passage will be stitched closed. If this is not necessary the remaining bowel will be closed off, leaving your back passage in place. You may then occasionally feel the urge to go to the toilet as you did before, and may occasionally pass mucus/slime into the toilet. This is normal and nothing to be worried about.
Urostomy
The tubes that carry urine from your kidneys to your bladder (ureters) are disconnected from your bladder and joined to a short piece of your bowel. Usually the small bowel is used but occasionally the colon can be used. This is then brought out onto the skin surface to create your urostomy. A urostomy is usually on the right hand side of your abdomen. A watertight bag with a drainable tap sticks over the urostomy to collect your urine.
The stoma care nurse specialist will contact you before your admission to hospital to give you more detailed information, including booklets about living with a stoma. You will be shown the type of bags you will need, and given contact details for any further information. You will see the stoma care nurse specialist in hospital before your operation to put marks on your abdomen. This acts as a guide for the surgeon. It is important to do this when you are awake so you are involved in identifying the most suitable place for your stomas.
Following your surgery, the stoma care nurse specialist will continue to see and advise you. She/he will support you until you feel you are able to look after your stomas with confidence.
Altered body image
Changes in bodily function and having stomas may affect how you see yourself and how you feel about your body. It is important that you talk to Mr Chattopadhyay and his team members about any aspects you find difficult to cope with.
Sexual function and sexuality
A cancer diagnosis can be very emotional and frightening. Often the symptoms you may initially have can affect the way you feel about yourself. If you are currently in a relationship, these reactions may cause a loss in sexual desire. This can be a worrying time for both you and your partner.
Following this type of surgery, as well as having two stomas formed, you may have your uterus (womb) and ovaries removed, as well as part or your entire vagina. This is necessary to aim to remove all the cancer. The surgery can also interfere with the nerve supply to your genitalia, and may affect your ability to achieve an orgasm. This may have an impact on your sexuality, and also on your sexual function.
Removal of your uterus (womb) and ovaries will mean a loss in fertility and your ability to have children. Removal of these organs will also mean that you stop your menstrual cycle and will start the menopause. This will have been discussed in detail with you before your operation.
If you have consented to have part or your entire vagina removed, and you strongly wish to remain sexually active, please ensure that you discuss these issues with Mr Chattopadhyay and his team. There may be a possibility in certain circumstances of making a new vagina in the future using other tissues in your body. All aspects of this type of surgery, and potential results will need to be discussed carefully.
If you are currently in a relationship, this can be a worrying time for your partner also. He or she should be encouraged to be involved in discussions about the operation and how it is likely to affect your relationship afterwards. There are alternative ways to achieve sexual pleasure, and you may need sexual rehabilitation following this type of surgery to explore these issues.
Before your operation – what to expect
Before your operation you will attend a pre-admission clinic to check a number of things in preparation for surgery.
You will have a MRSA (Methicillin Resistant Staphylococcus Aureus) test before admission to help your team and the nurses plan your care. This involves taking a simple swab of your nose, throat and perineum (seat area). This is a routine procedure carried out on all patients who are admitted to the hospital for surgery. You can get more detailed information on MRSA from the infection control team, or ask one of the nurses.
Other investigations to prepare you for the operation include blood, heart and lung tests. These tests will help us assess your fitness for surgery. Before your operation members of the team will visit you. These include surgeons, anaesthetists, and specialist nurses including a stoma care nurse specialist. When you feel you fully understand the operation and what is going to happen to you, you will be asked to sign a consent form.
You will be admitted the day before your operation, for a stay of approximately 14 to 21 days. The staff will give you bowel preparation to empty your bowel. You will be able to have ‘clear fluids’, for example black tea/coffee and squash, and we will encourage you to drink plenty of water. If you are unsure of what you can drink, please ask a member of the nursing staff. On the evening before your operation a fluid drip, given through a vein, may be put up to help keep you hydrated before your operation.
The nursing staff on the ward will do their best to tell you the time of your operation. The nurses will also tell you when to stop drinking in preparation of surgery. On the morning of your operation you will be asked to have a wash and get ready for theatre. Once you are ready, a nurse will accompany you to the operating theatre.
After your operation – what to expect
Following your surgery you will be cared for in the Intensive treatment/therapy unit or high dependency unit (ITU/HDU). You will be awake but under careful observation. You will see equipment that delivers drugs and monitors that display information about your blood pressure, heart rate and rhythm. The machines can be noisy, but please do not be worried since you are being continually observed.
Nursing in the ITU/HDU is usually on a ratio of one nurse to two patients, to provide the best support. The team will review you on a regular basis and when everything is stable, you will be transferred back to the main ward. The nurses will co-ordinate this and keep you and your family informed.
Pain relief
The anaesthetist will discuss your pain management with you before your operation. The two main pain relief options are an epidural (given via a fine tube inserted into your back) or a patient controlled analgesia (PCA is a painkiller via a drip into your vein).
A specialist pain team will review the best pain relief to help minimise any discomfort. By the time you are ready to leave hospital, simple painkilling tablets are effective, and they will be provided for you on discharge.
General care
After surgery, you will have a number of drips in place for fluids and drugs. These will be given to you through a vein. Following pelvic surgery, it can take time for bowel function to return (usually 5 to 7 days after the operation, sometimes longer). Throughout the period that your bowel is resting and recovering a drip (IV fluids) will be used to keep you hydrated. You can take sips of water to keep your mouth moist and comfortable.
Sometimes it may take longer for your bowel to recover, in which case liquid food (parenteral nutrition) will be provided through a drip. Once bowel activity shows signs of returning, you will be able to increase the fluids you take by mouth. This will gradually increase until you can manage a light diet.
To help prevent you feeling sick a tube may be placed in your stomach via the nose to drain any fluid in the stomach. This is called a nasogastric tube and is placed whilst you are asleep in theatre. It should not affect your ability to talk or breathe and will be removed once you are drinking.
Your abdominal wound is joined with stitches or staples (metal clips). The stitches are usually dissolvable and do not need to be removed. If you have clips, these are normally removed after 10 to 14 days. The nurses on the ward can do this, or district nurses if you have already returned home. If you have a perineal (back passage) wound, the stitches are usually dissolvable and do not need to be removed. If you have a skin flap, the stitches may not be dissolvable and are normally removed after 10 to 14 days.
When you have had an operation, it is normal for blood and fluid to be produced, so you may have a drain or tube in your abdomen to remove this fluid. The amount will be monitored and the tube will be removed when drainage decreases. Your nurse will remove the drain on the ward. These procedures are not painful, but can be a little uncomfortable. If you are at all worried, talk with the nursing staff.
During your stay, you will wear stockings called (TEDS). You will receive a daily injection of a blood-thinning agent (anticoagulant). The TED stockings and the injection help prevent blood clots forming in your legs. You will be discharged home with blood thinning injections (anticoagulants) for a period of time as discussed with you by your team (usually for 28 days after your operation).
If you have any questions at any time, ask any member of your team. They will be pleased to explain anything that concerns you or your family. Another good tip is to write your thoughts and questions down so that you do not forget.
Physiotherapy
Physiotherapy early after your operation can reduce the risks of a chest infection as well as preventing blood clots forming in your legs. Physiotherapy will start the day after your operation. The role of the physiotherapist is to work with you to help improve your lungs, and to increase your movement after surgery. Try to move around as soon as you can.
Counselling and psychological support
Patients and relatives may have difficulty in coping with illness, the effects of treatment and the effects of surgery on self-image, and may benefit from counselling and psychological support. As part of your care, your team will be able to discuss any issues or concerns you may have as a result of surgery.
Getting back to normal
Recovery time after surgery varies. You may find it takes weeks, sometimes months, to feel better; however, you can expect a gradual improvement over the next 6 to 12 weeks.