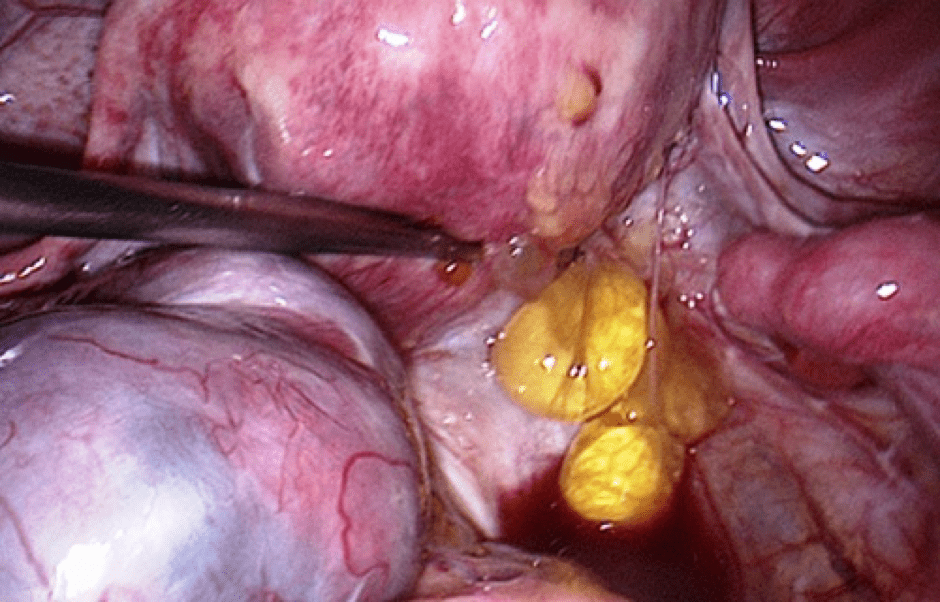
An image of a uterus showing endometriosis adhesions
Every month a woman’s body goes through hormonal changes. Hormones are naturally released which cause the lining of the womb to increase in preparation for a fertilized egg. If pregnancy does not occur, this lining will break down and bleed – this is then released from the body as a period. In endometriosis, cells like the ones in the lining of the womb grow elsewhere in the body. These cells react to the menstrual cycle each month and also bleed. However, there is no way for this blood to leave the body. This can cause inflammation, pain and the formation of scar tissue.
Endometriosis can have a significant impact on a woman’s life in a number of ways, including:
Chronic pain
Fatigue/lack of energy
Depression/isolation
Problems with a couple’s sex life/relationships
An inability to conceive
Difficulty in fulfilling work and social commitments
However, with the right endometriosis treatment, many of these issues can be addressed, and the symptoms of endometriosis made more manageable.
It’s important to remember that:
Endometriosis is not an infection
Endometriosis is not contagious
Endometriosis is not cancer
How is endometriosis diagnosed?
Getting diagnosed with endometriosis may take some time. The symptoms of endometriosis are very similar to other common conditions. It’s important to share as much information with your doctor as possible. It’s important to share as much information with Mr Chattopadhyay as possible.
The only definitive way to diagnose endometriosis is by a laparoscopy. If endometriosis is diagnosed, the endometriosis may be treated or removed for further examination during the laparoscopy.
Scans, blood tests and internal examinations are not a conclusive way to diagnose endometriosis and a normal scan, blood test and internal examination does not mean that you do not have endometriosis.
Because endometriosis manifests itself in a variety of ways and shares symptoms with other conditions, diagnosis can be difficult and often delayed. Recent research shows that there is now an average of 7.5 years between women first seeing a doctor about their symptoms and receiving a firm diagnosis.
How is endometriosis treated?
If you have been diagnosed with endometriosis, Mr Chattopadhyay will discuss possible endometriosis treatment options with you.
Currently, there is no cure for endometriosis. The different treatments available for endometriosis aim to reduce the severity of symptoms and improve the quality of life for a woman living with the condition. The type of treatment you receive for your endometriosis should be decided in partnership between you and Mr Chattopadhyay. Mr Chattopadhyay will consider many different factors when working out the best endometriosis treatment method for you, such as your age, the severity of endometriosis you have and the severity of your symptoms.
Mr Chattopadhyay may not recommend any particular treatment for endometriosis, but support you in seeking treatment options appropriate to your individual circumstances.
Treatment options available to women with endometriosis are:
Surgery
As a treatment for endometriosis, surgery can be used to alleviate pain by removing the endometriosis, dividing adhesions or removing cysts. There are two options of surgery for treating endometriosis:
Conservative surgery
Conservative surgery aims to remove or destroy the deposits of endometriosis and is usually done via a laparoscopy. Mr Chattopadhyay can either cut out the endometriosis (known as excision) or destroy it using heat or laser. Although surgery can provide relief from symptoms, they can recur in time.
Complex Surgery
Depending on the severity of your endometriosis, you may need to undergo more complex surgery that involves different organs within the body, such as the bowel or the bladder. These types of surgery will often include a multi-disciplinary team such as a colorectal surgeon, and are usually carried out via laparoscopy. Any complex surgery should be discussed thoroughly with Mr Chattopadhyay.
Radical surgery
More radical surgery can be considered if a woman has not responded to drug treatments or conservative surgery and is not planning to start a family. Radical surgery refers to a hysterectomy or oophorectomy.
Hysterectomy is the removal of the womb, and is performed under general anaesthetic. It can be done with or without removing the ovaries. If the ovaries are left in place then the chance of endometriosis returning is increased. Some women need a further operation to remove the ovaries at a later date. Hysterectomy is not the right operation for everyone and not a decision to make lightly. Consider all options and discuss things fully with Mr Chattopadhyay. Remember that a hysterectomy is irreversible.
Oophorectomy is the removal of the ovaries. When both ovaries are removed, the surgical procedure is called “bilateral oophorectomy,” whereas the removal of only one ovary is called “unilateral oophorectomy.” When both ovaries are removed, a woman will experience an instant and irreversible menopause.
These procedures may be considered for a number of reasons. The decision to have either of these procedures is a big one to make – they are irreversible, so the advantages and disadvantages of each surgery should be discussed in full with your consultant.
Hormone treatment
As endometriosis responds and grows when exposed to the female hormone oestrogen, a number of hormone treatments attempt to block or reduce the production of oestrogen in the body. This means the endometriosis will be unable to continue growing and will help to relieve symptoms.
If you are offered the choice of hormone treatment, you may want to discuss with Mr Chattopadhyay what the treatment involves, the pros and cons, along with the possible side effects of the treatment.
Hormone treatments for endometriosis either put you into an artificial pregnancy state or an artificial menopausal state. Both states are temporary and are reversed when you have stopped taking the hormones. Please note that these drugs have no effect on adhesions and neither do they help to improve fertility.
Mr Chattopadhyay will be able to discuss different hormone treatment options that are available to you.
The following hormone treatment options are available to women with endometriosis:
Combined oral contraceptive pill (‘the Pill’) https://www.endometriosis-uk.org/hormones#oral-contraceptive
Mirena Coil https://www.endometriosis-uk.org/hormones#mirena-coil
Progestogens https://www.endometriosis-uk.org/hormones#Progestogens
GnRH analogues https://www.endometriosis-uk.org/hormones#GnRH
Testosterone derivatives https://www.endometriosis-uk.org/hormones#Testosterone
Danazol https://www.endometriosis-uk.org/hormones#Danazol
Gestrinone (Dimetriose) https://www.evidence.nhs.uk/Search?ps=50&q=gestrinone
Pain relief
The main symptom of endometriosis is pelvic pain – there are various pain relief and pain management options available.
Heat and comfort
A simple hot water bottle or hot bath may help to reduce pain. Some women also find heated wheat bags to be effective.. Being comfortable and reducing stress will also be beneficial.
Painkillers
NSAIDs such as Ibuprofen, Voltarol and Ponstan (mefanemic acid) block the production of prostaglandins in the body. Prostaglandins occur naturally, in response to injury or disease, and cause pain and inflammation. They have a number of functions including making the womb contract during a period (which helps with the shedding of the womb lining). These contractions can cause pain. It is thought that women with endometriosis may produce more prostaglandins than women without the condition.
NSAIDs only work effectively if they are taken before the body produces prostaglandins. Many people take NSAIDs as they would other painkillers such as paracetamol. It is best to start taking NSAIDs the day before, or several days before, a period or pain is expected. Common side effects of NSAIDs include nausea, vomiting, diarrhoea, stomach upsets and stomach ulcers. These side effects can be reduced by taking the drugs with food or milk.
Codeine-based painkillers are effective painkillers but can cause constipation and gastro-intestinal upset, which may aggravate symptoms in women with endometriosis.
Simple analgesics such as paracetamol can be used to treat mild pain.
Physiotherapy
Physiotherapists can develop a programme of exercise and relaxation techniques designed to help strengthen pelvic floor muscles, reduce pain, and manage stress and anxiety. After surgery, rehabilitation in the form of gentle exercises, yoga, or Pilates can help the body get back into shape by strengthening compromised abdominal and back muscles.
Pain modifiers
These drugs work by altering the body’s perception of pain. Tricyclic anti-depressants (example – Amitriptyline) are drugs that are mainly used to treat depression but have been found to have an effect on the nervous system and the way the body manages pain. The pain messages travel through the body’s central nervous system, but these drugs can help to stop those messages from reaching the brain.
Pain clinics
Some hospitals and trusts have specialised pain clinics providing advice and support to people in chronic pain. Ask Mr Chattopadhyay about a referral to your nearest pain clinic.
Transcutaneous Electrical Nerve Stimulator (TENS) machines
TENS machines are an alternative to pain killers. They are small, unobtrusive machines with electrodes that attach to the skin and send electrical pulses into the body. This does not hurt but instead feels mildly ticklish. The electrical pulses are thought to work by either blocking the pain messages as they travel through the nerves or by helping the body produce endorphins which are natural pain-fighters. Some TENS machines can be clipped to a belt. Check with Mr Chattopadhyay before using a TENS machine as they are not suitable for those who may be pregnant or who have a heart condition.
https://www.endometriosis-uk.org/information