What Is Fibroid?
Fibroids are benign (non-cancerous) tumours (abnormal growth of tissue). They grow on or in the muscle layer of the uterus (womb). The medical name for fibroids is uterine leiomyomas. Doctors usually describe the size of a uterus enlarged by fibroids in the same way they talk about the size of a pregnant uterus. So when a fibroid stretches the uterus to a 12- to 14-week size, the uterus is about the same size it would be if you were 12 to 14 weeks pregnant. This refers to a fibroid about the size of a small melon, or to several smaller fibroids. Fibroids that are large enough to cause symptomsare usually felt when doing a routine pelvic examination. Fibroids may be discovered when you have no symptoms at all.
How many types are there?
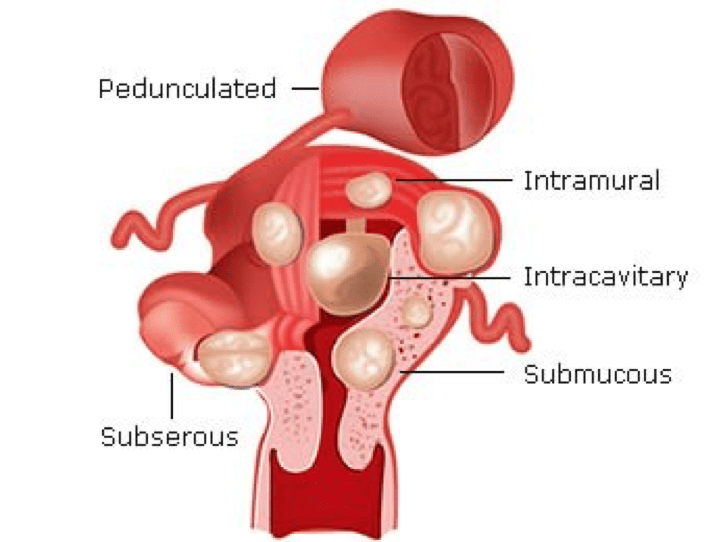
Fibroids can grow in different areas of the womb. Fibroids are classified according to their locations into 3 different types:
Submucosal
Under the lining of the womb, can grow on stalk (called pedunculated).
Intramural
Within the wall of the womb, most common type, may distort the uterine cavity, or cause irregular external uterine contour.
Subserosal
On the outer wall of the uterus and usually causes no symptoms until it grows large enough to cause interference to adjacent organs. Sometimes, they grow on stalk.
Fibroids may grow as a single tumour (growth) or in a cluster. A single fibroid can be size of a pea or quite large as a melon. A bunch or cluster of fibroids can also vary in size.
What are the risk factors?
There are no confirmed risk factors; however, it is known that fibroids are common in women of child bearing age (between 25 to 45 years of age). They are 2 – 3 times more common in Afro-Caribbean origin women and tend to be larger and more numerous. Women who are overweight or obese are at higher risk. Women who have given birth appear to be at lower risk.
What are the causes?
Little is known about the causes uterine fibroids. There are a number of theories, but none of these ideas gives a complete explanation. Most likely, fibroids are the product of many factors, which could be genetic, hormonal, environmental, or a combination of all three. After menopause, fibroids tend to shrink but may not disappear.
What are the symptoms?
Many women don’t have any symptoms and therefore you probably don’t even know you have fibroids. However, some women who have uterine fibroids may experience the following symptoms:
Summary of Symptoms
Prolonged and heavy bleeding or painful periods and bleeding between periods
- Flooding: a sudden gush of blood.
- Prolonged periods: much longer duration than you had in the past, e.g. 10 days compared to 4/5 days previously.
- Large blood clots, probably size of 50p coin or more.
These symptoms can be distressing, make you feel very tired and restrict your daily activities. You could be changing your tampons/pads every hours and find it difficult to go to work.
Anaemia
Heavy monthly bleeding can lead to iron deficiency which may you feel very weak, tired and dizzy.
It may be so severe to warrant at least iron level correction while waiting for a decision on the treatment of the fibroids.
Pain
Large blood clots or multiple fibroids cause severe pain & cramps. Large fibroids press on the lumbar and sacral nerve trunks to cause chronic pelvic pain. Pain during sex happens when the fibroids press on the cervix or they hang through the cervix into the vagina. Bleeding may also occur.
Pressure-related on adjacent organs
Large fibroids exert pressure on the nerve and blood vessels which can result in a dull ache in the thighs and varicose veins. Pressure from large subserous fibroid can cause the followings: Increase in frequency to pass urine. Leaking and dribbling of urine. Urgent need to pass urine but only small amount comes. In severe cases, difficulty or inability to pass urine may require a catheter. Occasionally, cystitis: caused by trapped urine which later becomes infected, constipation & haemorrhoids: caused by pressure on the rectum, lower back pain, constipation and haemorrhoids.
What are the complications of fibroids?
Fertility
Large fibroids affect fertility by: Impairing the lining of the womb. Compressing or obstructing the fallopian tubes. Distorting the shape of the womb cavity. Preventing sperm movement from reaching the womb.
Pregnancy
Multiple fibroids, particularly those in the lower part of the womb, can block the vagina during pregnancy and therefore a caesarean may be necessary for delivery. Risk of miscarriages is increased with the presence of multiple fibroids. Pain & premature labour can happen when fibroids degenerate (die) during pregnancy.
Urinary Tract Infection
Pressure exerts by the fibroids on the bladder can lead to urinary tract infection and on the urethra can result in urinary obstruction and kidney dysfunction.
Fibroid growth in other organs
Fibroid rarely breaks away from the womb and when it does, you can get: BML (Benign Metastasing Leiomyoma) in the lungs. Disseminated Peritoneal Leiomyomatosis in the abdominal wall. Neither condition is cancerous.
Cancer
Only very rare that fibroid develops into cancer but there is 0.2% risk of malignant transformation (i.e. becoming cancerous).
How is fibroid diagnosed?
If the fibroids are large enough to cause symptoms, Mr Chattopadhyay can feel them by pelvic examination. Sometimes, they bulge out from your lower abdomen even if you don’t have symptoms.
To confirm diagnosis, Mr Chattopadhyay will organise an ultrasound scan, a hysteroscopic examination, an MRI or a CT scan.
Ultrasound scan
There are two types of ultrasound used for diagnosis of fibroids:
Abdominal Pelvic
This uses a probe. The sonographer applies a “cold” gel on your tummy then presses the probe to the abdomen to get an image. Before the scan, you will be asked to drink up to 1 litre of water, hold it and only empty the bladder after she/he finishes the scan.
Transvaginal
This uses a wand which is inserted into the vagina to produce an image. This type of scan should be painless unless there is a large fibroid causing abdominal tenderness which makes you feel some discomfort.
Hysteroscopic examination
A procedure to look inside the womb under local or general anaesthetic. Mr Chattopadhyay inserts a tiny telescope that is attached to a camera into the vagina.
A picture is shown on the monitor. At the same time, Mr Chattopadhyay may look for polyps and also take a small sample of the lining of the womb for testing.
This test is often used together with an ultrasound scan to confirm diagnosis.
MRI and CT
These techniques will only be used when the ultrasound scans have not given a clear result or when a more detailed information is required.
Treatment Options Summary
In most cases, fibroids do not cause any symptoms and do not interfere with pregnancy and therefore no treatment is required.
In case of mild symptoms, Mr Chattopadhyay may consider no treatment but to monitor to see if they are growing.
Treatment is only warranted when the fibroids are large which interfere with pregnancy or fertility and cause symptoms.
The choice of treatment is highly individual and tailored to individual circumstances. There are important factors (see table) that you must consider and convey clearly to Mr Chattopadhyay so that in consultation you and him can agree on an appropriate treatment. They include questions below:
Do you have any symptoms?
Do you want to become pregnant?
Your age, e.g. are you near menopausal age?
What is the size of the fibroid(s)
Location of the fibroid(s).
In principle, a particular chosen treatment aims to achieve either [1] or [2], and in most cases (most women’s wishes) both of the followings:
- The management of abnormal uterine bleeding (AUB) which relieves symptoms of menorrhagia, anaemia, pelvic pressure effects (renal tract-urethra, bladder) and pelvic pain.
- An attempt to improve fertility (reducing the risk of miscarriage).
Available treatment options for fibroids are summarised in the table below and the choice is mainly governed by the woman’s fertility wishes: