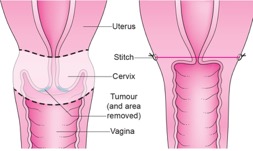
The part of the cervix that is removed during the surgery is checked under a microscope, often while you are still in the operating theatre. If there are no cancer cells around the edge of the tissue that has been removed and your surgeon is sure that all the cancer has gone, you will not need to have any more tissue removed.
If the lab results show that some cancer has been left behind, you will have to have more tissue taken away. Your surgeon may then have to do a hysterectomy after all. This can only be done during the same operation if you have given your consent beforehand. Some women may have combined chemotherapy and radiotherapy (chemoradiation) instead of hysterectomy.
Lymph nodes
Once all the checks have been done, Mr Chattopadhyay will put in the stitch that will hold your cervix closed. Because there is a small risk of cancer spread to the lymph nodes in stage 1B cancers and some stage 1A cancers, Mr Chattopadhyay may also need to remove some lymph nodes from around your womb.
After surgery
Your final results will be discussed in the gynaecological cancer multidisciplinary team meeting (MDT) at the Leicester Royal Infirmary.
The lymph nodes will be checked under a microscope to see if they contain any cancer cells. If they don’t, then you will not need any further treatment. If cancer cells are found in any lymph nodes, it is a sign that some cancer cells could have escaped from your cervix and a cancer could begin to grow again.
Mr Chattopadhyay is then likely to suggest that you have some radiotherapy to kill off any other cancer cells that may have been left behind. If you need to have radiotherapy, you will not be able to have a baby after the treatment. This can be very upsetting if you were hoping to have a family. Your medical and nursing team will do all they can to support you.
How you might feel
Radical trachelectomy is a small operation. You will usually only have to be in hospital for 2 or 3 days. Most women recover very quickly and complications are uncommon.
Possible risks
Possible risks and complications from this surgery are:
- Bleeding during or after your operation – this may need to be treated with a blood transfusion
- Infections – you will be given antibiotics during and after surgery to help prevent this
- Blood clots (deep vein thrombosis or DVT) – we will ask you to wear special stockings and to have daily blood thinning (anticoagulant) injections after your operation to prevent this
- Generally making a slow recovery
- Problems caused by having a general anaesthetic
- Also there is a risk that a small hole can develop in the bowel, if this occurs, the injury will be repaired at the time of operation.
Risks specific to this type of surgery include:
Lymphoedema – may occur when the lymphatic drainage system becomes blocked and surrounding tissues may swell, causing swelling in the lower body and legs. This can lead to skin problems, pain and discomfort. This can become permanent and can happen months or even years after surgery. Some early research suggests that this will affect less than 5 in 100 of patients having this procedure.
Lymphocysts or lymphoceles – these are swellings filled with fluid that develop in your abdomen after your operation. They are often naturally re-absorbed by your body, but if they are larger or causing you discomfort, your surgeon may drain them by using local anaesthetic and a needle.
Bladder problems –a small number of women will have difficulty emptying their bladder after this surgery and may need to go home with a catheter in their bladder for several weeks. A very small number of women may have long-term difficulties with emptying their bladder, but this is rare.
Problems with menstruation (your periods) – some women may find that the blood from their menstrual cycle (monthly period) becomes trapped inside the womb as the entrance is too small for it to drain away fully. If this happens, you will need to have a minor surgical procedure to open the entrance to the womb during a minor surgical procedure.
These complications are usually rare but you must be aware of them. As with any operation, there is some risk of death, although this is also rare. Please talk to your doctor about any concerns you have before your operation.
Mr Chattopadhyay will make sure the benefits of having a radical trachelectomy outweigh these possible risks.
Follow up
You will have a follow up appointment after your surgery. At your first follow up appointment, Mr Chattopadhyay will give you the results of the surgery, examine you and ask how you are and if you’ve had any problems. This is also your opportunity to ask any questions. Write down any questions you have before your appointment to help you remember what to ask. Taking someone with you can also help you to remember what Mr Chattopadhyay says. How often you have follow up appointments and for how long depends on the results of your surgery.
Surgery to remove the womb (radical hysterectomy)
Surgery to remove the womb is quite a big operation, and may be necessary to make sure that all the cancer has gone.
What happens
During the operation, the surgeon will remove your womb, all the tissues holding your womb in place, the top of your vagina and all the lymph nodes around the womb. This is called a radical hysterectomy (or Wertheim’s hysterectomy).
Before surgery
Ovaries
If you have had your menopause, your doctor will talk to you about taking out your ovaries as well. They are not usually affected by the cancer, but some surgeons think it is a good idea to take them out and remove your risk of getting ovarian cancer in the future.
It is important to know that you are at no higher risk of cancer of the ovary than any other woman in the general population.
If you have not had your menopause, it may be possible to leave the ovaries because removing them would put you into an early (premature) menopause. If your ovaries do have to be removed, you may need to take hormone replacement therapy (HRT) to prevent menopausal symptoms and the effects of the menopause on your bones and other body organs.
After surgery
You will be in hospital for between 4 and 7 days and recovering at home afterwards for at least another month or so.
Possible risks
As with any operation there are risks and complications which can occur but it is important to remember these risks are uncommon.
The anaesthetist will discuss the risks associated with general anaesthetic and your pain control after surgery.
You will have some blood loss at the time of your operation. A blood transfusion may be necessary to replace blood lost during the operation in about 1 in 5 women. On very rare occasions there may be internal bleeding which will require a second operation.
Occasionally you may develop blood clots in the veins of the legs or pelvis; these clots can sometimes travel to the lungs. To minimise the risk of this we give you injections to thin the blood and try to get you to move around as soon as you are able following your operation.
The physiotherapist will also visit you both before and after your operation to encourage an early return to normal activity.
Also there is a small risk of developing an infection which may be in the chest (3 in 100) wound (5 in 100), pelvis (4 in 100) or urine (10 in 100). To reduce this risk you will be given an antibiotic just before the start of the operation. Wound breakdown rarely occurs in 5 in 1000 women needing to return to theatre for resuturing of the wound.
There is a risk that a small hole can develop in the bladder, or in the ureter (tube which carries urine to the bladder) this may require further procedure to correct either at the time of the operation or at a later date. Also there is a risk that a small hole can develop in the bowel if this occurs the injury will be repaired at the time of operation.
With any type of operation there is a very small risk of death.
During your operation, a catheter is inserted into the bladder (through your abdomen), to drain off the urine. The catheter is usually left in for at least five days. It can take several weeks before your bladder begins to work properly again, and changes in bladder sensation and function may be permanent. The nurses can teach you to catheterise yourself to help with your bladder management.
Rarely, women experience swelling in the legs or lower abdomen (lymphoedema). Sometimes patients experience numbness around the scar area and the top and outside of the legs this is due to damage of the small nerves. This may resolve with time.
There is a small risk of fluid collection where the lymph glands were removed from the pelvis; this is called a (lymphocyst). This may resolve on its own with time, however, it can be easily managed by either draining or a surgical procedure.
Follow up
You will have a follow up appointment after your surgery. At your first follow up appointment, Mr Chattopadhyay will give you the results of the surgery, examine you and ask how you are and if you’ve had any problems. This is also your opportunity to ask any questions. Write down any questions you have before your appointment to help you remember what to ask. Taking someone with you can also help you to remember what Mr Chattopadhyay says. How often you have follow up appointments and for how long depends on the results of your surgery.