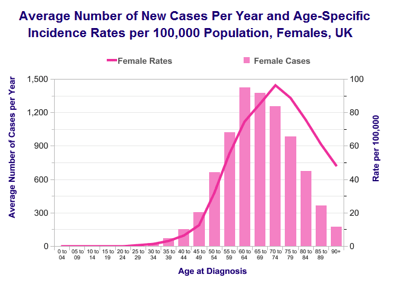
- 8,600 new cases per year in UK
- 22 cases per 100,000 women per year in UK
- Life time risk in general population is 1 in 41
- Life-time risk in mutation carrier is 1 in 2
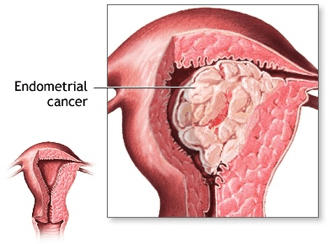
- Most uterine cancers are endometrial cancers and they are diagnosed in early stage.
- Most common gynaecological cancer in UK
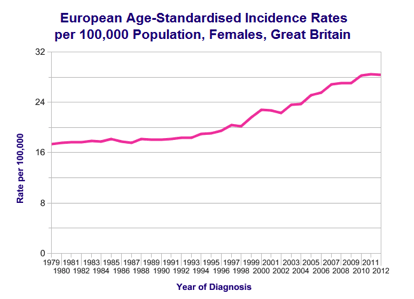
- Incidence rates have increased since 1970s
Risk factors and Causes
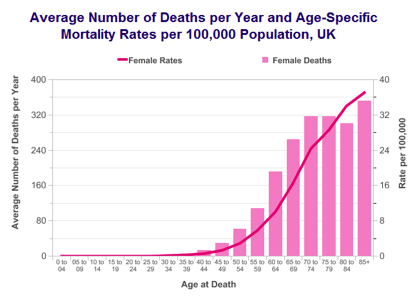
- Age
- High BMI and obesity
- High parity, contraceptive pills (Reduces risk by reducing number of menstrual cycles)
- Early menarche and late menopause
- HRT
- PCOS
- Tamoxifen
- Lynch syndrome mutations
- Diabetes and hypertension
- Strong family history
- Previous bowel cancer
Screening
There is no population screening programme to prevent endometrial cancer. Research using ultrasound scan to check for thick endometrial lining shows some promise but results are not yet sufficiently convincing to establish a population screening programme for endometrial cancer. Benefit of such screening in improvement of survival is not entirely clear.
Women with strong family history of lynch syndrome genetic mutation or associated cancers are at very high-risk of developing endometrial cancer. They are usually offered hysterectomy after completion of family. Meanwhile they may benefit from screening with ultrasound scan, Pipelle endometrial sampling or hysteroscopy at regular interval. They may also benefit from progesterone releasing intra-uterine devices such as Mirena ® IUS (Coil).
Risk of endometrial cancer can also be reduced by healthy life style, weight management and by using combined oral contraceptive pills.
Symptoms
- Irregular vaginal bleeding
- Bleeding in-between periods
- Post-menopausal bleeding
- Chronic vaginal discharge
- Weight loss
- Bladder or bowel problems
- Leg swellings
- Bone pain
Investigations
For Diagnosis
- Pipelle endometrial biopsy
- Hysteroscopy guided endometrial biopsy
For Staging
- CT Scan
- MRI
- PET CT Scan
FIGO Stage
Stage 1 – Cancer is limited to uterine body either to inner half (A) or growing more than half way towards surface of womb (B)
Stage 2 – Cancer has spread locally to cervix
Stage 3 – Cancer has spread outside uterus but limited in pelvis, involving surface of uterus, ovaries or fallopian tubes (A), vagina or parametrium (tissue around uterus) (B) or lymph nodes (C)
Stage 4 – Cancer has spread to bladder or bowel (A) or other body parts such as lung, liver, bone or brain (B)
Treatment
Treatment of uterine cancer is mainly with surgery.
If there is no evidence of spread of cancer outside uterus (FIGO Stage 1), women are usually treated with laparoscopic (key-hole) full hysterectomy and removal of both tubes and ovaries. If the grade (how aggressive cell look under microscope) of cancer is high, some centres also perform pelvic lymph node removal to check for cancer spread in lymph node and guide radiotherapy. Some woman in this approach will have negative lymph nodes (so did not benefit from having it removed). Whilst other centre may not perform routine lymph node removal but based on tumour characteristics offer radiotherapy. Some women in this approach will have negative lymph node and therefore unnecessary radiotherapy. New technology of sentinel node detection in time will help establish uniform strategy in the surgical management of endometrial cancer.
FIGO Stage 2 uterine cancers are also treated in similar fashion to Stage 1 but may require radical hysterectomy and removal of top of vagina.
Some women with node negative FIGO Stage 1 or 2 cancers may be offered brachytherapy (internal radiotherapy) based on risk factors to reduce local recurrence. Women with positive nodes are recommended to have both External Beam Radiotherapy and Brachytherapy.
Radical hysterectomy can be offered in small number of selected cases of FIGO Stage 3 but most of these women will also require Radiotherapy, Chemotherapy or both.
Women with FIGO Stage 4 uterine cancer are usually treated with chemotherapy first. Those with very good response to chemotherapy may become suitable for further treatment with Radiotherapy, Surgery or both.
Women suitable but not fit for surgery may be offered palliative chemotherapy or hormonal treatment with radiotherapy reserved for symptom control.
Survival
Survival in uterine cancer mainly depends on the
- FIGO stage of the cancer (how far has cancer spread)
- Grade of cancer (how aggressive cancer cell look under microscope)
- Morphology (cell type) of cancer
- Age
- Fitness of patient
In general at least 84 out of 100 women with uterine cancer will live 5 years or more.
- Stage 1 – 95 out of 100 will survive 5 years or more (95%)
- Stage 2 – 77 out of 100 will survive 5 years or more (77%)
- Stage 3 – 39 out of 100 will survive 5 years or more (39%)
- Stage 4 – 14 out of 100 will survive 5 years or more (14%)
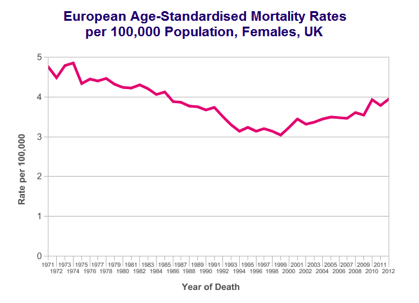
Overall survival in uterine cancer has improved gradually over last four decades.
Further Information and Support
http://www.cancerresearchuk.org/about-cancer/womb-cancer/living-with/resources-organisations


