What are the symptoms of pelvic inflammatory disease (PID)?
Pain in the lower tummy (abdomen), called the pelvic area, is the most common symptom. It can range from mild to severe.
Other symptoms that may also occur include:
Abnormal vaginal bleeding, which occurs in about 1 in 4 cases. This may be periods that are heavier than usual, or bleeding between periods, or bleeding after having sex.
Pain during sex.
Abnormal vaginal discharge.
High temperature (fever).
Low back pain.
Symptoms may develop quickly. You can become quite ill over a few days. Sometimes symptoms are mild and develop slowly. For example, you may just have a mild abdominal pain that may ‘grumble on’ for weeks. In some cases no symptoms develop and you do not know that you are infected. However, you are still at risk of complications even if you have no symptoms at first.
Who gets pelvic inflammatory disease (PID)?
About 1 in 50 sexually active women in the UK develop PID each year. It most commonly develops in women aged between 15 and 24 years. The risk of developing PID is higher if you have had:
A recent change of sexual partner. The risk goes up with the number of partners.
A previous episode of PID or sexually transmitted disease.
A recent abortion.
A recent operation or procedure on the womb (uterus).
A contraceptive coil inserted recently.
What tests may be done?
If pelvic inflammatory disease (PID) is suspected, a small sample of discharge (a swab) is usually taken from the neck of your womb (cervix). This is to test for any germs (bacteria). A swab from the urethra (where you pass urine from) and blood and urine tests may also be taken. These are to look for infecting bacteria or the effects of infection.
Sometimes the swabs and tests may not show any bacteria. So to help confirm a diagnosis of PID, other tests may be needed. For example, an ultrasound scan may be able to show inflamed Fallopian tubes. Other scans are sometimes done.
If Mr Chattopadhyay has particular concerns, he may need to look inside your tummy (abdomen) to see your womb (uterus) and tubes. Whilst you are under general anaesthetic a thin telescope (laparoscope) is pushed through your tummy wall. This is called a laparoscopy. Laparoscopy is not routinely needed to diagnose PID.
PID may not be diagnosed for some time if symptoms are mild, or do not occur at first.
A pregnancy test is also usually done in women suspected of having PID. This is because an ectopic pregnancy can sometimes be confused with PID, as some of the symptoms are similar. An ectopic pregnancy is a pregnancy that develops in a Fallopian tube and can cause serious problems.
What are the possible complications?
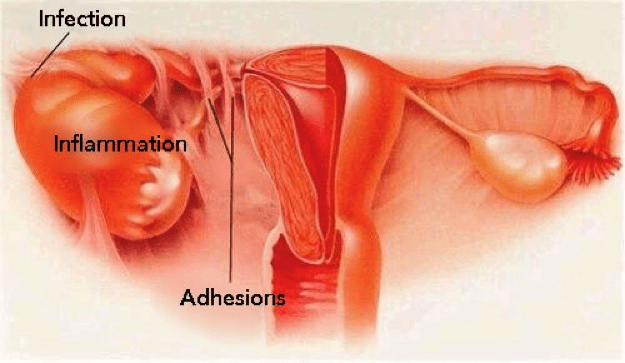
Complications do not develop in most cases if pelvic inflammatory disease (PID) is diagnosed and treated early. Possible complications include one or more of the following:
Difficulty becoming pregnant (infertility). PID can cause scarring or damage to the Fallopian tubes. This can occur whether or not the PID caused symptoms.
An increased risk of a pregnancy developing in a Fallopian tube (an ectopic pregnancy) if you become pregnant. This is due to damage to the Fallopian tube by the infection. If you have had PID and become pregnant, you have about a 1 in 10 chance that it will be ectopic.
Persistent pain may develop. This often includes pain during sex.
The risks of developing some complications of pregnancy (such as miscarriage, premature birth and stillbirth) are increased in pregnant women with untreated PID.
Reiter’s syndrome. This is an uncommon cause of arthritis and eye inflammation. It is an uncommon complication of PID. It is thought to be due to the immune system ‘over-reacting’ to pelvic infection in some cases.
A collection of pus (an abscess) sometimes develops next to the womb (uterus) if the infection is severe.
You are less likely to develop complications if you begin treatment within 2-3 days of symptoms starting. This may be possible if symptoms develop quickly. However, some women with PID have mild symptoms, or no symptoms at all. The infection may progress for quite some time before it is diagnosed or treated.
What is the treatment of pelvic inflammatory disease (PID)?
The usual treatment is a course of antibiotics for at least two weeks. Sometimes Mr Chattopadhyay may feel you need to be in hospital for treatment. This is advisable if your temperature is very high (higher than 38°C) or there are signs of a collection of pus (an abscess).
Two different antibiotics are usually prescribed. This is to cover the range of possible germs (bacteria) that can cause PID. It is important to take the full course of treatment. Treatment will usually be started as soon as possible if PID is suspected. This might sometimes be even before the results of samples (swabs) or other tests are available. This is because the earlier the treatment, the better the outlook, and the lower the risk of future fertility problems.
Please let Mr Chattopadhyay know if you are (or may be) pregnant. This may affect the choice of antibiotic.
Occasionally, an operation is needed. For example, to drain an abscess if one develops (which is very uncommon).
You should not have sex until both you and your sexual partner have finished treatment.
Does my partner need to be treated?
Yes. Also, any other sexual partner within the previous six months should be tested for infection. If you have not had sex within the previous six months then your latest sexual partner (however long ago the relationship was) should be tested and treated. A course of antibiotics is usually advised whether or not infection is found on testing.
This is because:
The majority of pelvic inflammatory disease (PID) is caused by chlamydia. It is often passed on during sex.
Men often have no symptoms with chlamydia, but can still pass on the infection.
The test for chlamydia is not 100% reliable. Treatment makes sure that any possible infection which may have been missed by the tests is cleared.
If your sexual partner is infected and not treated, chlamydia may be passed back to you again after you are treated.
Can pelvic inflammatory disease (PID) be prevented?
Wearing a condom during sex helps to protect you from sexually transmitted infections. The risk of infection increases with the number of changes of sexual partner.
If you are sexually active and under 25 years old, you should be tested for chlamydia every year or when you change your sexual partner. There are lots of local places where you can get a test – young peoples clinics, youth clubs, colleges, contraception/family planning clinics, your GP surgery, sexual health (genitourinary) clinics and some pharmacies. The test is simple and painless. It is totally voluntary and completely confidential. You can take the test yourself and you do not need to be examined. You will be asked to give a urine sample or, in some places, to take a sample (swab) from the lower vagina (a cotton wool bud is used to wipe the area).
Will it happen again?
About 1 in 5 women who have pelvic inflammatory disease (PID) have a further episode. This is usually within two years. Reasons why this may occur include:
If your sexual partner was not treated. You are then likely to get the infection back again.
If you did not take the antibiotics properly, or for long enough, the infection may then not clear completely, and may flare up again later.
If you change your sexual partner and do not practise ‘safer sex’ by using condoms.
Some women are more prone to infection once their womb (uterus) or tubes have been damaged by a previous episode of PID.
The risk of developing complications such as infertility or persistent pelvic pain is greatly increased with repeated episodes of PID.
https://patient.info/health/pelvic-inflammatory-disease-leaflet