The time it will take you to recover from surgery will depend on the type of surgery and how extensive it was. For extensive operations, such as a pelvic exenteration, it may be many weeks or months before you start to feel better.
Mr Chattopadhyay will talk to you about the possible risks associated with the type of procedure you’re having. Possible risks include infection, bleeding, blood clots, altered sensation in your vulva, and problems having sex.
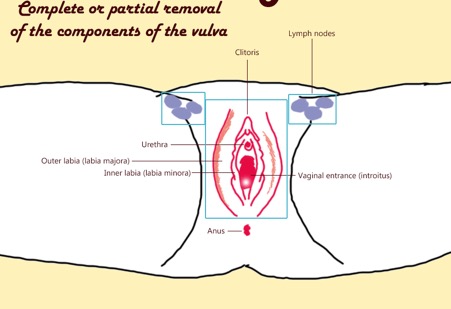
Assessing and removing groin lymph nodes
An additional operation may also be required to assess whether the cancerous cells have spread into one or more lymph nodes in your groin, and remove these if they’re found to contain cancer. This may involve one or more of the procedures outlined below.
Sentinel node biopsy
If the cancer has spread to nearby lymph nodes, it’s sometimes possible to only remove certain lymph nodes, known as sentinel nodes.
Sentinel nodes are identified by injecting a dye at the site of the tumour and studying its flow to locate the nodes closest to the tumour. These are then removed and checked for cancerous cells. This is offered by Mr Chattopadhyay in the NHS only.
Groin lymphadenectomy
In some cases, some or all of the nodes in your groin may need to be surgically removed. This is called a groin or inguino-femoral lymphadenectomy. Further treatment with radiotherapy may also be recommended.
Removing cancerous lymph nodes reduces the risk of the cancer returning, but it can make you more vulnerable to infection and cause swelling in your legs from a build-up of lymphatic fluid (lymphoedema).
Pelvic exenteration
In cases of advanced vulval cancer or where the cancer returns after previous treatment, an operation called a pelvic exenteration may be recommended. This involves removing your entire vulva as well as your bladder, womb and part of your bowel. This is a major operation and isn’t carried out very often these days.
If a section of your bowel is removed, it will be necessary for your surgeon to divert your bowel through an opening made in your tummy (a stoma). Stools then pass along this piece of bowel and into a bag you wear over the stoma. This is known as a colostomy.
If your bladder is removed, urine can be passed out of your body into a pouch via a stoma. This is known as a urostomy. Alternatively, it may be possible to create a new bladder by removing a section of your bowel and using it to create a pouch to store urine in.
Mr Chattopadhyay does this operation with colorectal surgeons and urologists.
Reconstructive surgery
If only a small amount of tissue has been removed during surgery, the skin of the vulva can often be neatly stitched together.
Otherwise, it may be necessary to reconstruct the vulva using a skin graft, where a piece of skin is taken from your thigh or tummy and moved to the wound in your vulva. Another option is to have a skin flap, where an area of skin near the vulva is used to create a flap and cover the wound.
These reconstructive procedures are usually carried out at the same time as the operation to remove the cancer.
Mr Chattopadhyay does this operation jointly with plastic surgeons.
After your operation
When you wake up, you may have a drip in place to give you fluids until you are eating and drinking again. You may be given antibiotics through the drip to help prevent any infection in your wound. You should be able to eat and drink as soon as you have got over your anaesthetic and the drip can then come down.
You may have a tube into your bladder (catheter) put in while you are in theatre. Depending on the operation you’ve had, this may only stay in overnight. Or you may need it in for a longer period of time. The catheter will drain urine from your bladder. You won’t have to go to the toilet or use a bedpan and the tube will stop urine from coming into contact with your wound.
If you have had lymph nodes removed from one or both groins, you will probably have a tube called a drain coming out of each groin wound. This is to drain fluid that collects in the area and helps to prevent swelling and infection. These drains will have to stay in until no more fluid is coming out. The time this takes varies and the drain may stay in for up to 14 days.
Your wound
You may or may not have a dressing covering your wound. Some surgeons prefer to leave the wound uncovered so that it can be regularly cleaned with warm sterile water. Your nurse will do this for you. Other surgeons like the wound to be kept covered for a few days. If you do have a dressing, your nurse will change it and clean the wound every few days at least.
If your wound is healing slowly, you may have to stay in hospital for longer than you originally thought. Or you may be able to go home and have a district nurse come in to take care of it. If you do go home, you will have to have someone there to help you manage.
The stitches used in vulval surgery are often soluble, so you don’t have to have them taken out. Sometimes they don’t dissolve and then do have to be removed. This won’t be done until the area has healed – at least 10 days.
Painkillers
The vulva is a sensitive area and your wound is bound to be sore at first. There are many different types of painkilling drugs you can have. It is important to tell your doctor or nurse as soon as you feel any pain. They need your help to find the right type and dose of painkiller for you. Painkillers work best when you take them regularly.
When you first wake up, you may have a pump containing painkillers attached to your drip. You may have a hand control from the pump with a button to press to give yourself extra painkillers, as you need them. This is called PCA or patient controlled analgesia. Do use it whenever you need to. You can’t overdose because the machine is set to prevent that. Do tell your nurse if you need to press the button very often. You may need a higher dose in the pump.
Some hospitals use painkillers given into the spine (an epidural) for the first day or so after surgery. These work very well. A very thin tube will be taped to your back. It will be connected to a pump that can give you a continuous dose of painkiller.
Whatever method of pain control you are having, tell your nurse if you are in pain. You may need a different type of painkiller, or a higher dose.
Getting over your surgery
If you have had a small operation, you should get over it quite quickly. If you have had a bigger operation, obviously it will take longer to recover. You should allow at least 6 weeks getting over it. Do bear in mind, though, that it takes longer than that for some women to recover. If it is taking you a while, you aren’t doing anything wrong. Some people just heal more quickly than others. Talk to your surgeon or nurse specialist at your 6 week follow up appointment if you are at all concerned.
This is an awkward place to have surgery. You will find moving around difficult at first. It is a good idea not to walk too much for the first few weeks, as this will put a strain on the healing wound and can be painful. Keep doing the leg exercises you learned while you were in hospital to help prevent blood clots.
You may find it better to lie propped up on your side, rather than try to sit. An air cushion can make sitting more comfortable. You should try to only sit on your wound for short periods of time.
To keep the area clean and as comfortable as possible, you could try
Having short warm baths as often as you like – don’t put any perfumed bath products, soap, creams, lotions or talc on the wound area
Rinsing your vulval area after passing urine by pouring a jug of warm water over while you are sitting on the toilet
Using a hairdryer on a cold or cool setting to dry the area instead of a towel
Taking a stool softener, such as lactulose, to make sure you don’t get constipated
Your wound will probably heal without any other problems. But if you develop oozing, a discharge that smells, heavy bleeding or have increasing pain, contact your doctor straight away. You may have an infection and need antibiotics.